Special report on a 10 year old girl with Atrial Septal Defect
Thank you very much for everyone's kind and encouraging comments about Camp Braveheart. These are well appreciated and strengthen my personal resolve to continue Operation Braveheart even after Rotary funds are exhausted. We can make this happen with everyone's continued support.
Friday, February 10, 2023 was an extra-special day for me in the Philippines. Before our anticipated trip, I asked Dr. Jonas to schedule a patient for repair while I was there. I wanted to touch base with him again and to bring some Rotarians and an undergraduate student over to experience transcatheter repair live.
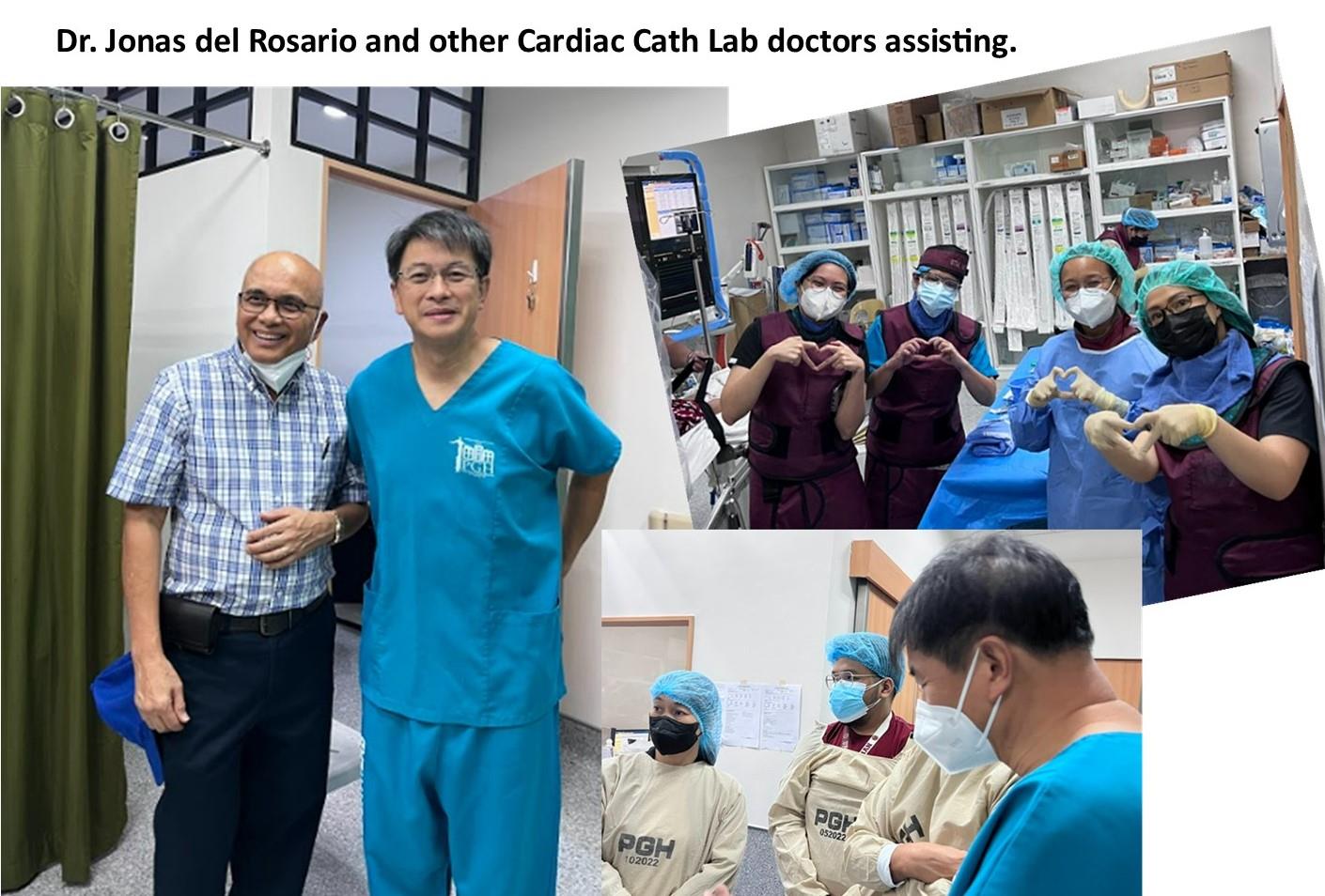
Together with three fellow Rotarians from the Rotary Club of Makati Southeast, we spent the morning at the cardiac cath lab in the Philippine General Hospital.(PGH) Past President Emmie picked me up in my hotel. She had experienced this before. The other two, Juliet and Maria came separately for a first time experience with transcatheter repair. Dr. Jonas del Rosario had to delay the 10 year old girl with Atrial Septal Defect (ASD) because of an emergency. He had to open up a blocked hole in a newborn baby's heart. He explained to us that transcatheter intervention not only SEALS holes in the heart defects but also opens up blocked holes.
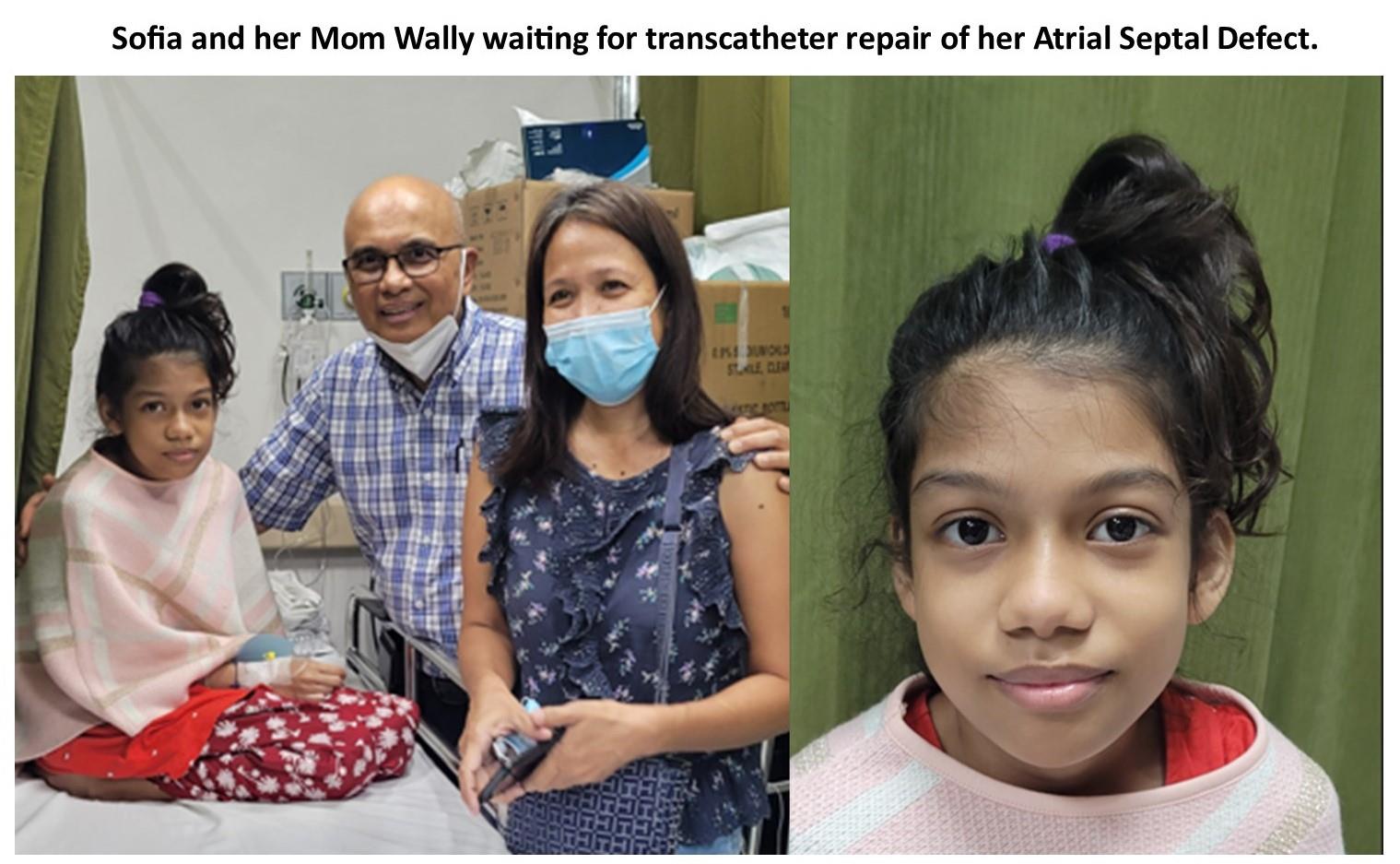
SOFIA, the scheduled Braveheart III patient, is a 10 year old girl from Pampanga (about two hours from PGH). Her mother, Wally, an unemployed preschool teacher, is a single mom. For the past four years, she had been actively and desperately seeking the help of doctors and medical institutions in the Metro Manila area. While in one of these hospitals, she noticed the name of Dr. Jonas listed on the directory. She bravely contacted Jonas who offered to see her and Sofia right away. To her pleasant surprise, Jonas scheduled Sofia for repair the next week. She couldn't believe it. After 4 years waiting and hoping, her daughter will finally be repaired immediately after she consulted with Jonas. It was sort of a shock and too soon for her to process that she started having second thoughts.
When I met Sofia and Wally at the PGH cardiac cath laboratory, both expressed fear and hesitation. Because of the delay we were able to have a lengthy conversation with Sofia and Wally. Transcatheter repair is not without possible complications. I assured Wally that Dr. Jonas had done thousands of these procedures and was the most skilled interventionist with the longest experience in the Philippines. Their fears were allayed when Jonas came in to tell them not to worry, everything will turn out fine.
Atrial septal defect (ASD) is a more complicated condition for repair. The device Jonas uses costs double the amount that is spent for the usual Patent Ductus Arteriosus (PDA). But thanks to all of you, our donors and the Rotary match, we have funds available for the device that Jonas will use to cure Sofia.
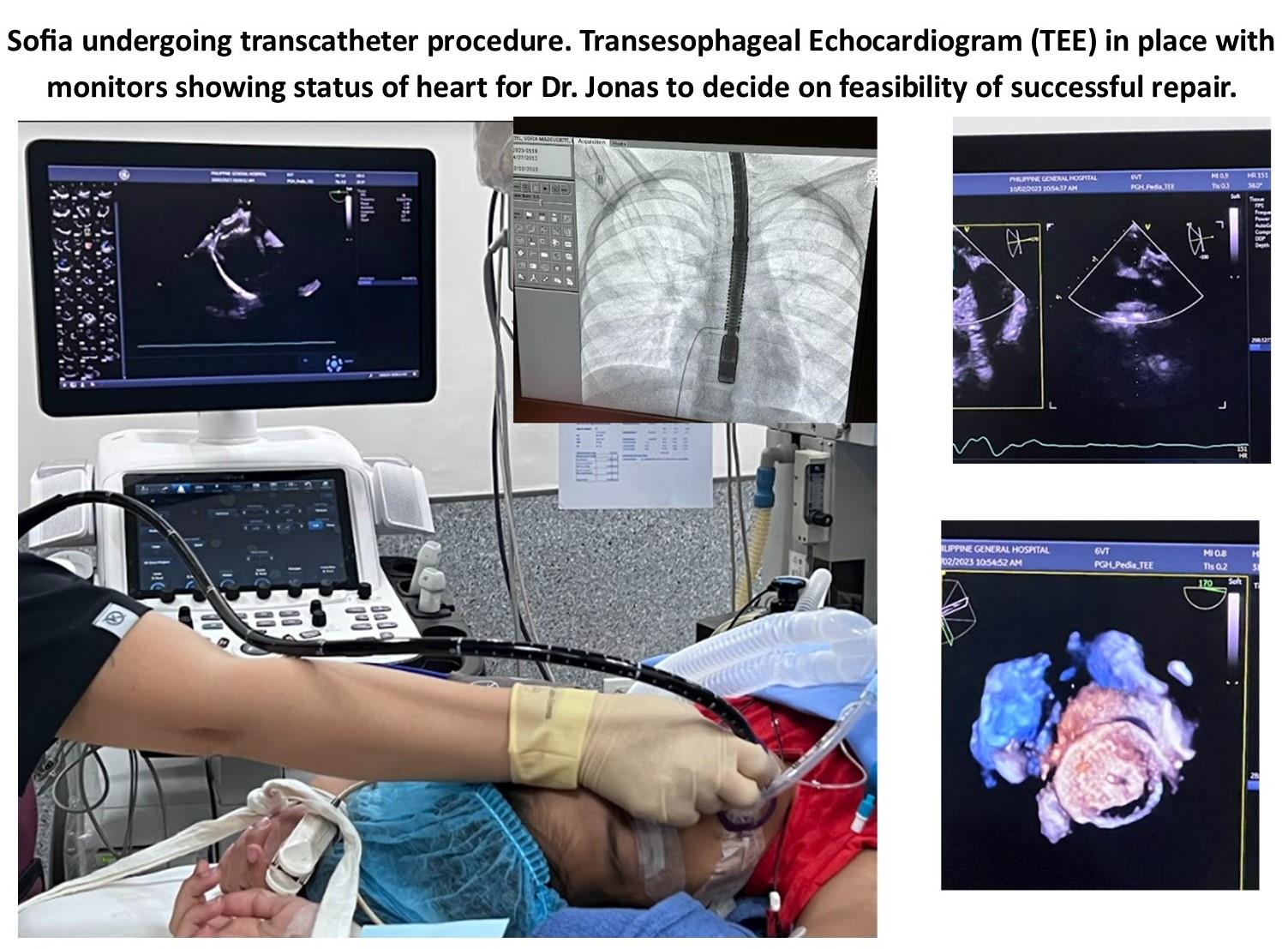
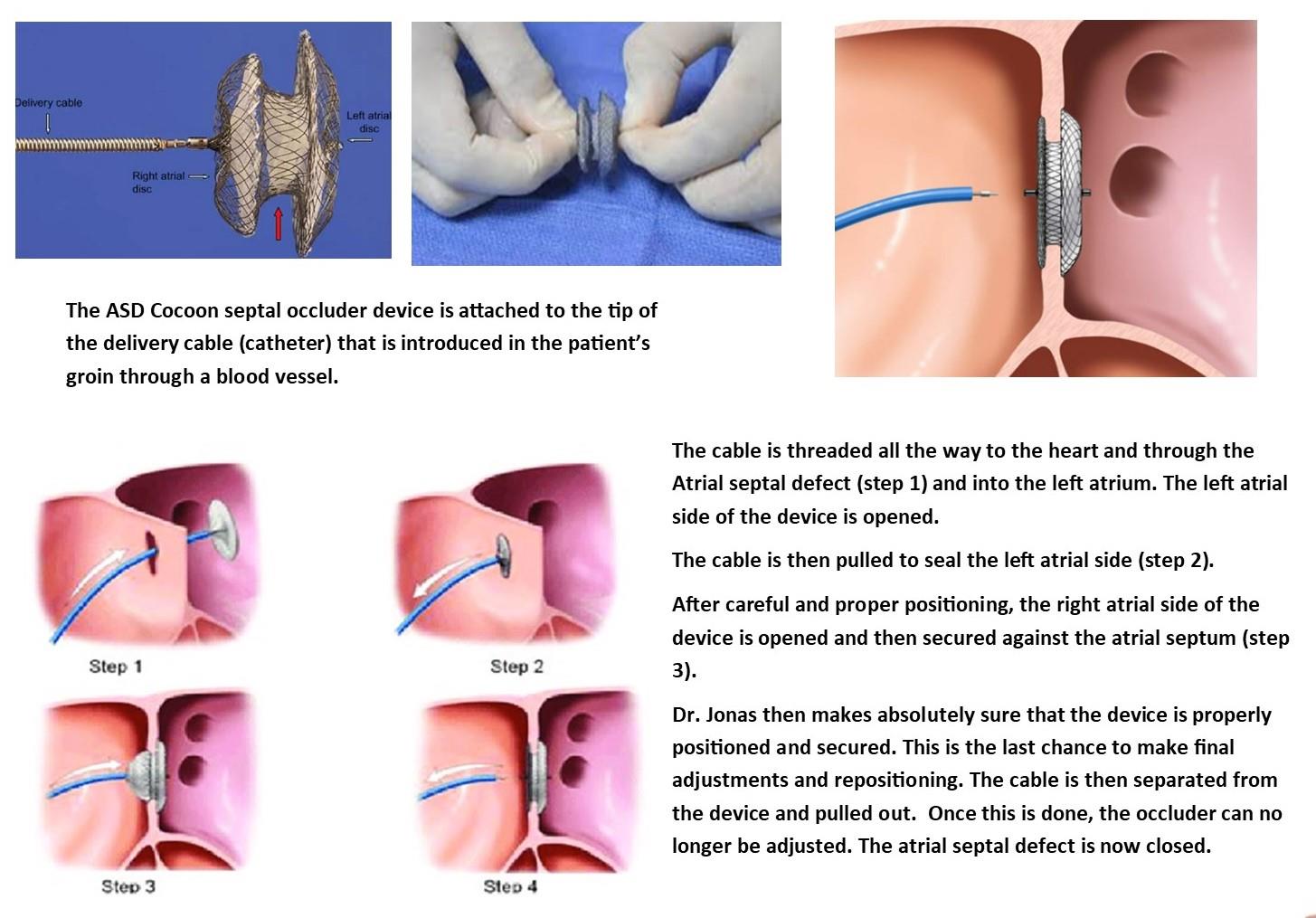
Sofia had to be anesthetized to allow the insertion of a tube through her mouth and down her esophagus in order for Jonas to visualize in computer monitors the condition of the defect with a TEE (transesophageal echocardiogram). Apparently, about 30% of ASD's can not be repaired with this procedure. Jonas had to insure that he had enough tissue for the device to be properly implanted and permanently secured. The device has to securely latch onto the soft tissue surrounding the septal defect for this to work. Otherwise, an open repair has to be done. Dr. Jonas came back to us with the good news and explanation that indeed, Sofia's ASD was amenable for repair.
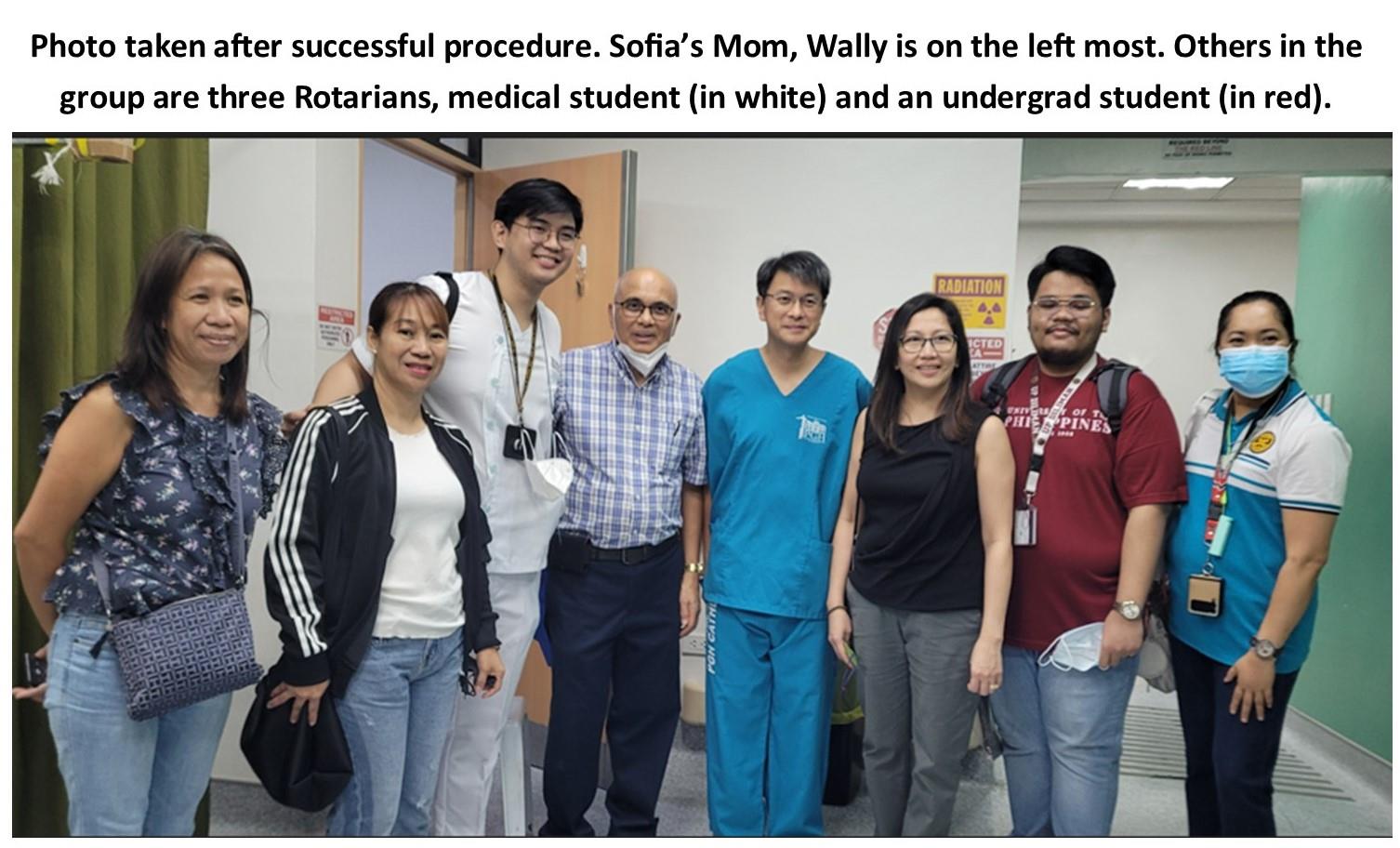
We watched the procedure from beginning to end. Also present were three other Rotarians, an undergraduate Biology (PreMed) major from UP Diliman and a third year medical student, my PHI fraternity brother who had been helping out with patient photos and demographics all along. We were all eyes during the procedure, concentrating on the TV monitors to view the catheter inserted, the device carefully deployed, accurately positioned, checked several times before finally released. The device placement must be perfectly done because once the device is released from the catheter, it can no longer be adjusted. The same applies to PDA closure.
There were four other physicians assisting in the procedure. When I asked them if they were willing to volunteer in the future when Jonas can no longer do this, they all replied without hesitation and in unison with a resounding YES. This made me feel confident that Operation Braveheart can continue long after the Rotary grant money is all spent.
After photos and goodbyes, we made a courtesy call to Dr. Gap Legaspi, Director of the Philippine General Hospital. Dr. Gap has been supportive from the start of this project. He allowed Operation Braveheart the access and use of the Cardiac cath laboratory at no cost. I reminded Dr. Gap that Braveheart III is the last Global Grant from Rotary but I am personally committed to continue the project even after Rotary funds are exhausted. Because of this, he intends to institutionalize Operation Braveheart in PGH so this courtesy can be extended after he leaves office and indefinitely.
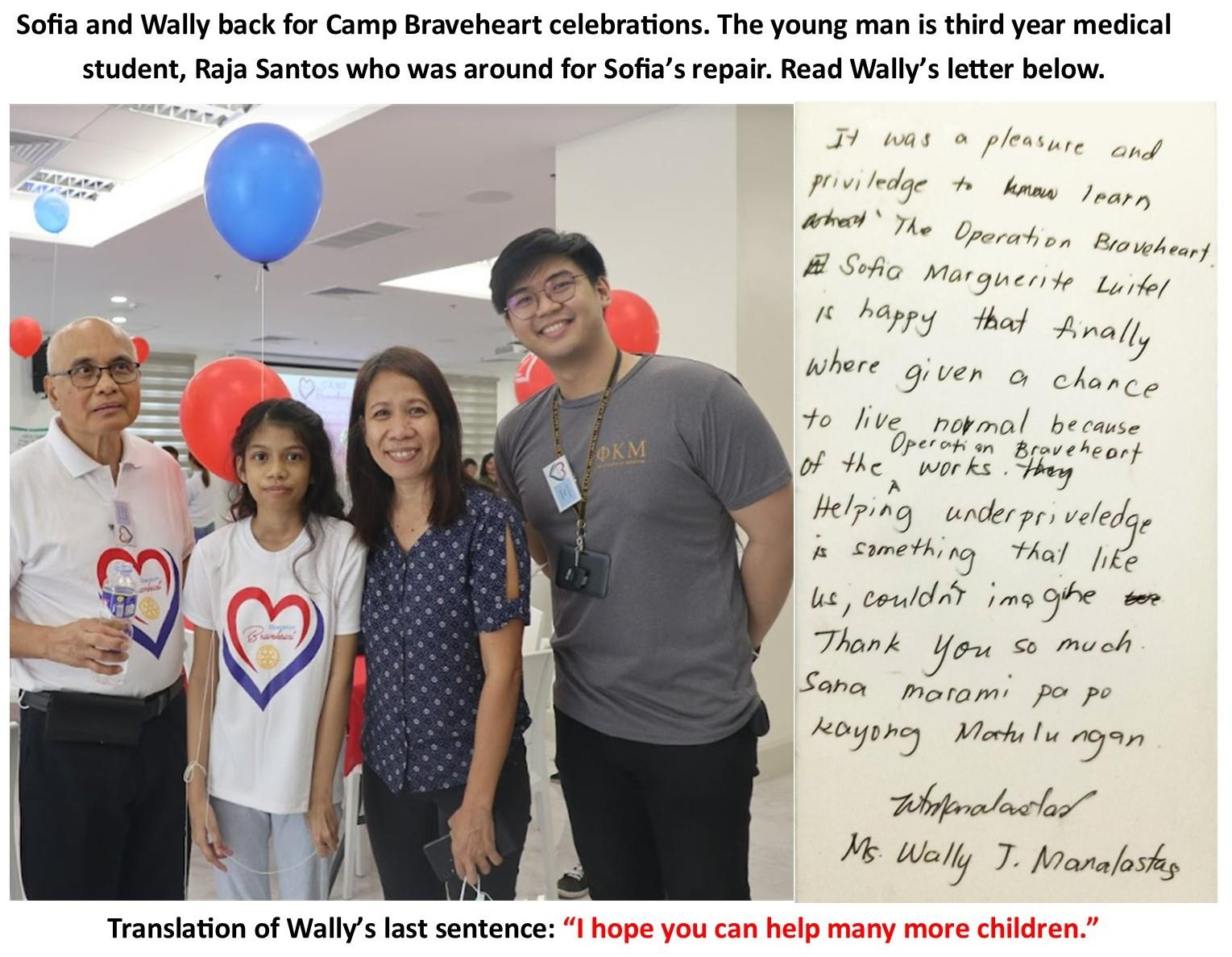
A week later, Sofia and her Mom Wally, no longer apprehensive, joined the Camp Braveheart celebrations.
Sofia's ASD repair is the 21st for Operation Braveheart III.
As of today, Operation Braveheart has facilitated the transcatheter repair of 180 patients (34 were ASD's).
Thank you very much for your continued support.
Jess Socrates, M.D., Coordinator Operation Braveheart